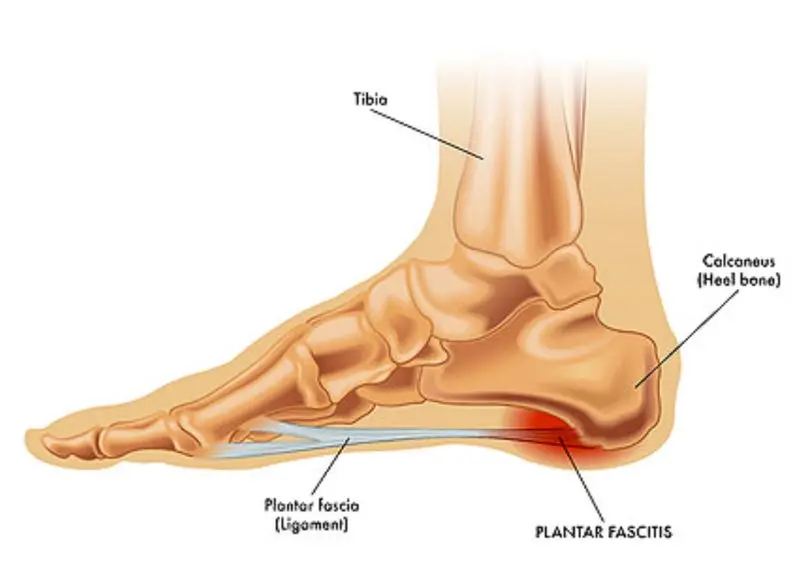
Waking up and placing your feet on the floor, only to be met with a sharp, stabbing pain in your heel, can make the simplest task feel daunting. This discomfort is often a hallmark of plantar fasciitis, an inflammation of the thick band of tissue connecting your heel bone to your toes.
To treat it effectively, you first need to understand exactly where the pain occurs and why it develops. Identifying the specific plantar fasciitis pain location is a critical first step toward building a treatment plan that works for your lifestyle.
In this detailed guide, we’ll explore where plantar fasciitis pain is typically felt, the common symptoms that accompany it, the causes behind the condition, and both at-home and medical treatments that can help you return to walking comfortably.
The Most Common Plantar Fasciitis Pain Location
For most people, the pain is concentrated at the bottom of the heel, right where the plantar fascia ligament attaches to the heel bone. This location is the primary site of inflammation and is often the most tender area when pressed.
Where Plantar Fasciitis Pain Starts
This is considered the defining feature of plantar fasciitis. You may notice pinpoint tenderness on the bottom-inside part of your heel. Applying gentle pressure with your thumb often recreates the discomfort. This sharp pain is usually most intense first thing in the morning or after long periods of rest, as the fascia has tightened and becomes less flexible.

Other Areas Where Pain May Appear
Although the heel is the most common location, pain can also extend along the arch of the foot. In some cases, the discomfort radiates forward toward the mid-foot. It’s important to differentiate this from heel spur pain, which stems from a bony growth. Plantar fasciitis pain comes from inflammation in soft tissue, not bone
Other Key Symptoms to Watch For
Knowing the exact pain location is only part of the picture. Plantar fasciitis typically comes with a cluster of recognizable symptoms that make the condition easier to identify.
Severe Pain with the First Steps
One of the hallmark signs is intense heel pain when you first stand up after rest, especially in the morning. During sleep, the fascia naturally shortens and tightens.
The moment you take those first steps, the sudden stretch can cause tiny micro-tears in the tissue, resulting in a sharp, stabbing pain. For many people, this “morning pain” is the most distressing symptom of plantar fasciitis.
Pain That Improves, Then Returns
You may notice that the discomfort lessens once you begin walking or moving around. This happens because gentle activity warms up the fascia, making it more flexible.
However, after long hours of standing, walking long distances, or engaging in strenuous activity, the inflammation flares up again. This cycle of relief followed by a return of pain is a common pattern in plantar fasciitis.

Varying Pain Types
The pain doesn’t always feel the same. Sometimes it’s a sharp, stabbing sensation that makes each step difficult; other times it lingers as a dull, nagging ache.
The intensity often shifts depending on your activity level, how long you’ve been on your feet, and the degree of inflammation present. This variation can make plantar fasciitis confusing to track and easy to mistake for other foot issues.
Causes of Plantar Fasciitis Pain
Plantar Fasciitis is a condition where the thick band of tissue running across the bottom of your foot, connecting your heel bone to your toes, becomes inflamed. This happens when repeated strain overloads the ligament, leading to small tears and inflammation in the fascia.
High-Impact or Repetitive Activity
Certain types of physical activities can put excessive stress on the heel and arch, making this injury more likely. The repeated impact can cause micro-tears in the plantar fascia that, over time, lead to chronic inflammation and pain.
- Long-Distance Running: The constant pounding from running places significant stress on the heel and arch of the foot with every stride, increasing the risk of developing plantar fasciitis.
- Aerobic Workouts and Dancing: Activities that involve repeated jumping and landing, such as high-impact aerobics or certain dance styles, can overload the fascia and lead to injury.
- Standing for Long Periods: People in professions that require them to stand or walk on hard surfaces for extended periods (like factory workers, nurses, or teachers) are also at a higher risk because of the constant pressure on their feet.
Foot Structure
The natural shape and structure of your foot play a crucial role in how weight is distributed. When this structure is not ideal, it can place additional strain on the plantar fascia.
- Flat Feet (Low Arches): When you have flat feet, the arch of your foot collapses or flattens when you walk, which overstretches the plantar fascia with each step.
- High Arches: Conversely, feet with very high arches are unable to absorb shock effectively. This can put a concentrated amount of stress on the heel and forefoot, causing the plantar fascia to tighten and strain.
Other Contributing Factors
- Sudden Weight Gain: Increased body weight adds more pressure to the foot’s structure.
- Unsupportive Footwear: Shoes lacking proper arch support or heel cushioning can worsen the condition.
- Extended Standing: Occupations that require hours of standing on hard floors increase the risk.
Diagnosis and Effective Treatment
Recognizing your symptoms and pain location is the first step. The next step is confirming the diagnosis and starting treatment.
Getting a Diagnosis
A healthcare provider can often diagnose plantar fasciitis through a physical examination. They will check for tenderness in the specific heel area and may assess your foot flexibility. Imaging, such as an X-ray, can rule out fractures or identify heel spurs.
At-Home Treatment Methods
- Rest and Ice: Reduce activities that aggravate your heel and apply ice for 15–20 minutes several times a day.
- Stretching: Gentle daily stretches for your calf muscles and plantar fascia can improve flexibility and reduce pain.
- Supportive Footwear: Choose shoes with firm arch support and cushioning, and consider orthotic inserts for added stability.

Advanced Treatment Options
If symptoms persist, doctors may recommend:
- Physical therapy to strengthen the surrounding muscles
- Corticosteroid injections to reduce inflammation
- Extracorporeal shockwave therapy (ESWT) to stimulate healing
Surgery is rarely required but can be considered for severe, unresponsive cases.
Expert Advice and Real-Life Experiences
Addressing plantar fasciitis early is crucial to preventing chronic pain. Timely intervention means faster recovery and a better chance of avoiding long-term complications.
“I used to wake up dreading that first step,” says John, a taxi driver from Aberdeen. “It was so painful, I thought I might have to quit work. With daily stretching and better footwear, I can now start my day without wincing.”
Conclusion
Understanding the precise plantar fasciitis pain location—and how it connects to your symptoms—allows you to make informed decisions about treatment. By combining self-care strategies, supportive footwear, and professional guidance when needed, you can significantly improve your chances of a full recovery.
Don’t let heel pain keep you sidelined. Identify the cause, take proactive steps, and get back to moving without discomfort.


